Have you ever experienced hoarseness or voice loss? There can be numerous reasons behind these conditions. According to feedback from ear, nose, and throat (ENT) specialists, approximately 50-78% of patients with voice disorders actually suffer from laryngopharyngeal reflux (LPR), commonly known as throat reflux. It’s been a journey of more than three months, filled with misdiagnoses from doctors and numerous detours. In this blog post, I will provide you with valuable information about LPR and share my personal recovery process.
Experiencing Dry Throat, Cough, and Difficulty in Producing Sound
Here’s my treatment record:
Silence Begins and Persistent Cough
On November 30th, my voice started to fade away, leaving me puzzled and concerned.
By December 3rd, a dry cough accompanied my voice loss, intensifying my worries.
Seeking Medical Help
Visiting a clinic on December 3rd, I was diagnosed with pharyngitis and prescribed a cough suppressant. My cough improved, and my voice returned to about 70-80%. Unfortunately, it didn’t last long, and I soon lost my ability to speak again.
Ineffective Nebulization Treatment and Traditional Chinese Medicine Diagnosis
From December 15th to December 17th, I underwent three nebulization treatments, hoping for a recovery. Sadly, they proved ineffective.
On December 25th, I sought a diagnosis from a Traditional Chinese Medicine hospital. They identified vocal fatigue and performed two acupuncture sessions, along with herbal medicine for my throat. Unfortunately, these treatments had little to no effect.
Laryngoscopy
On January 13th, a laryngoscopy revealed that my vocal cords were corroded by gastric acid, a crucial finding that was initially overlooked by doctors. Despite the new information, the diagnosis remained vocal fatigue and chronic pharyngitis, and the Chinese herbal medicine continued to be administered, yielding no improvement.
Surprisingly, on January 21st, my voice suddenly returned to around 80%. However, I soon caught a cold, experienced a hoarse voice, and developed a cough.
Discovering Laryngopharyngeal Reflux
During research on January 30th, I stumbled upon symptoms identical to mine: laryngopharyngeal reflux. Confirming my suspicions, I retrieved my previous laryngoscopy report. With dietary adjustments and refraining from eating three hours before bedtime, my voice started to improve.
On February 13th, after a long presentation, my throat felt fatigued, and my condition worsened. Seeking medical help again on February 27th, I began taking medication for my stomach. Mosapride (enhances gastric motility) 5mg x 3 and Nexium (acid suppressant) 20mg x 2. There was some improvement, but I experienced bloating after every meal.
Silence as the Best Medicine
Beginning on March 5th, I decided to enforce complete vocal rest to aid my recovery. By March 8th, the bloating in my stomach had diminished, providing some relief.
With my voice gradually improving, I persisted with the regimen of vocal rest. On March 12th, I noticed further improvements in the clarity and strength of my voice. The silent treatment was proving to be an essential component of my recovery.
Unexpected Setbacks, Pain and Declining Voice
Unfortunately, in the early hours of March 13th, I experienced a sudden bout of acute gastroenteritis, characterized by vomiting and diarrhea. The previous night’s meal, which consisted of a pear, was the likely culprit. Despite this setback, I remained determined to overcome the challenges.
As days passed, my voice gradually regressed, accompanied by stomach discomfort on March 16th. The frustration grew, as it seemed like a never-ending cycle of setbacks and progress.
Taking matters into my own hands, I sought treatment from a gastroenterologist on March 18th. The prescribed regimen included Itopride (digestive medication), magnesium aluminum carbonate chewable tablets, and Nexium (acid suppressant).
Stepping Away from Accutane
On March 21st, I made the decision to discontinue the use of Accutane, a medication previously prescribed to me. Unfortunately, my voice suffered another setback on March 28th. Speaking became increasingly difficult and painful, leaving me disheartened and searching for answers.
My recovery is still ongoing. For these months of road to recovery, I have done some research during my road to recovery. Let me share some with you:
Research for Myself
Incidence Rate
“From an epidemiological standpoint, LPR is one of the most frequently encountered chronic inflammatory conditions of the larynx, affecting 8–20 % of the general population, 4–10 % of patients in Ear Nose and Throat (ENT) consultation, 1 % of patients in primary care practices and up to 75 % of patients with refractory ENT symptoms.
LPR may concern 50–78 % of the population with voice complaints and 91 % of the cases of voice disorders in the elderly.
For many practitioners, hoarseness is considered the main symptom, present in 65–95 % of LPR subjects. Hoarseness generated by inflammation and/or vocal fold lesions can lead to functional complaints, including vocal forcing, forcing sensations, vocal fatigue, musculoskeletal tension, and hard glottal attacks.”
Source: Voice outcomes of laryngopharyngeal reflux treatment: a systematic review of 1483 patients
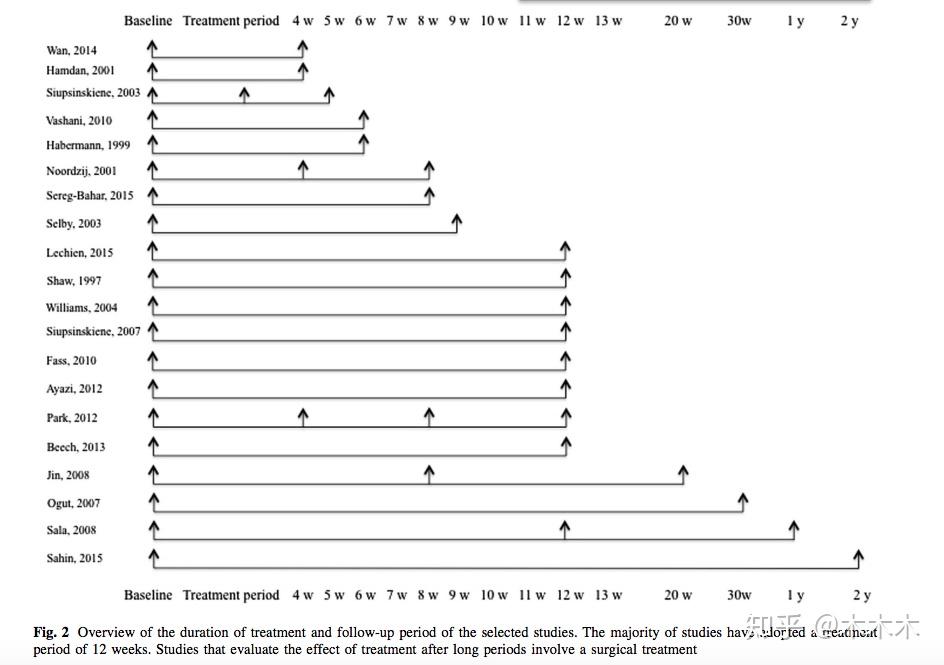
Duration and Results of Voice Restoration Treatment
If you’re considering voice restoration treatment, it’s essential to understand that noticeable results typically take at least four weeks or more to appear. The treatment process involves a series of sessions, and during this time, your vocal cords will undergo healing and repair. Patience and consistency are key as you embark on this journey towards vocal recovery.
As the treatment progresses, you will experience gradual improvements in the health of your vocal cords. The goal is for your voice to return to its normal range and quality, allowing you to communicate effortlessly and confidently once again. It’s important to note that each individual’s response to the treatment may vary, so results may manifest at different rates.
“Method: Aryngopharyngeal reflux patients were treated medically and voice analysis was conducted three times: before treatment, 1 to 2 months after treatment, and 3 to 4 months after treatment. Jitter, shimmer, and harmonic-to-noise ratio (HNR) were analyzed as the acoustic parameters. Pre- and posttreatment reflux symptom index and reflux finding score were documented.
RESULTS: Jitter, shimmer, and HNR had improved significantly at 1 to 2 months after treatment and were maintained at 3 to 4 months after treatment. Jitter was significantly correlated with reflux symptom index.”
Effectiveness of Vocal Rest and Medication in Treating Voice Disorders
Studies have shown that combining vocal rest with medication can lead to more favorable results in treating voice disorders. While the ideal duration of vocal rest has yet to be definitively determined, research suggests that an average vocal rest period of 8.8 days is effective. However, it is important to note that the specific duration of vocal rest required varies from case to case, and doctors often rely on their expertise and judgment.
Animal studies have shed light on the approximate recovery time for vocal cords. Typically, it takes around 5-7 days for vocal cords to begin the healing process, while post-surgery recovery may take a minimum of 14 days. These findings underline the importance of providing adequate rest to the vocal cords for optimal recovery.
“The average duration of recommended voice rest is on the order of a week in the postoperative setting. In a study by Rousseau et al., the mean duration of voice rest was 8.8 days. Vocal rest or restraint may also result in dysphonia due to deconditioning or pathology due to a change in vocal mechanics. Singing voice therapy has been demonstrated to benefit singers, the duration of treatment and the criteria for a handoff between speech-language pathologists in the rehabilitative setting and singing voice specialists or singing teachers in the habilitative setting is evolving.
The mean duration of voice rest was 8.8 days (range, 3-28), and the median was 7 days. Overall compliance was 34.5%.
Perhaps even more striking is the lack of empirical evidence supporting the use of vocal restrictions and/or voice rest. Unfortunately, this has led to disparate recommendations with regard to voice rest in clinical practice. For example, complete voice rest may be recommended for anywhere between 3 and 14 days following the removal of a vocal polyp, with some otolaryngologists unlikely to recommend any type of vocal restriction. Yet, the overall impact of voice rest on patient compliance and self-reported QOL remains unknown.”
Source: Healthcare for the Vocal Performing Artist
Restoring Vocal Cords
Avoid straining your voice by refraining from shouting, whispering, or singing loudly. Limiting your use of vocal cords and allowing them to rest will expedite the recovery process.0 Keeping your vocal cords hydrated is essential for their recovery. Drink plenty of water throughout the day to ensure your vocal cords remain lubricated. Avoid excessive caffeine and alcohol consumption as they can dehydrate your vocal cords. You can also use a humidifier or steam inhalation to add moisture to the air you breathe, providing relief to your vocal cords.
“Although the wound-healing process is not complete, collagen production begins and reepithelialization occurs between 5 and 7 days in animal models of vocal fold injury.
Yet, the question of whether voice rest should be restricted to 1 week remains controversial. In fact, 1 animal study reported that voice rest of at least 2 weeks after surgery may be needed to allow for complete restitution of the basement membrane.8 Ironically, as already mentioned, the most common duration of voice rest in clinical practice among otolaryngologists is 7 days.4 With the dearth of empirical data on effects of voice rest on vocal fold wound healing, the lack of consensus over the duration and type of voice rest is not surprising. Unfortunately, with the current lack of evidence to support voice rest recommendations, it is likely that some patients are receiving an inappropriate duration of voice rest for optimal healing.”
Source: Compliance and Quality of Life in Patients on Prescribed Voice Rest
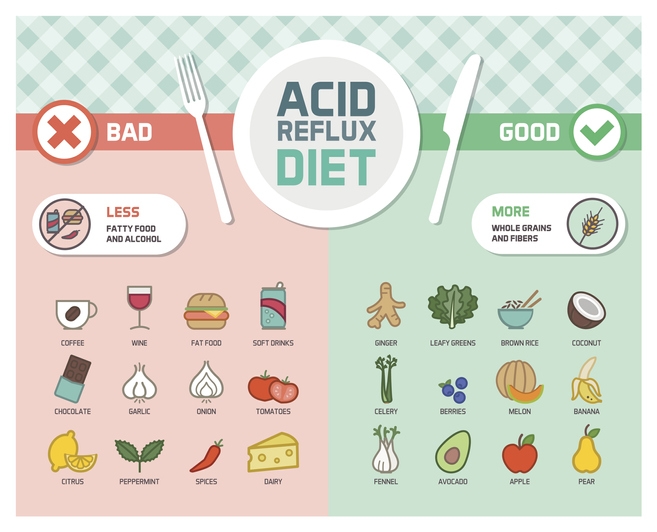
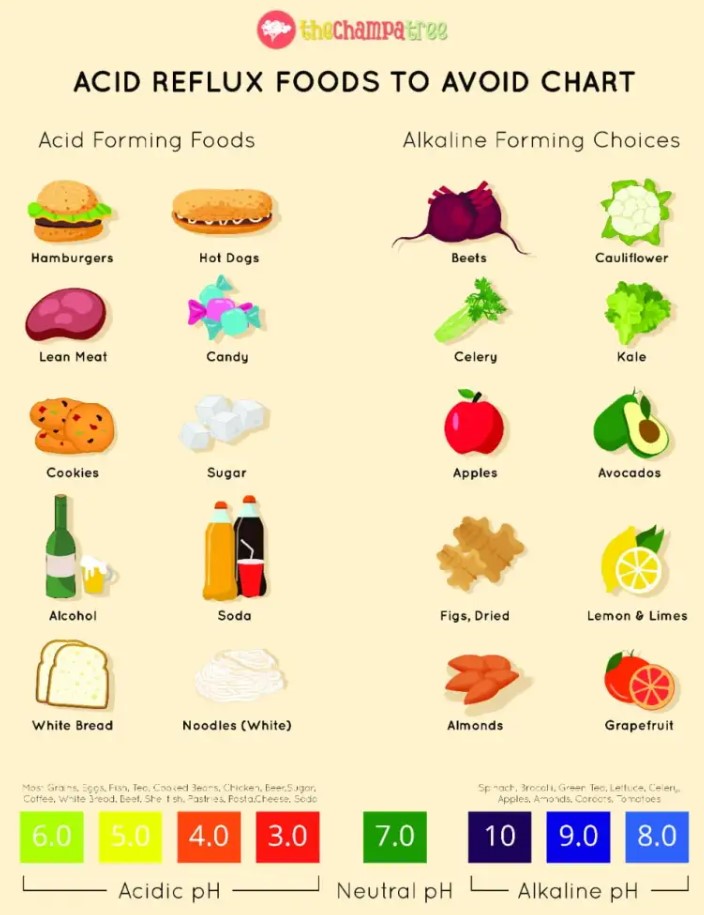
Food Lists for Acid Reflux Patients (Laryngopharyngeal Reflux)
External Reference
- Voice outcomes of laryngopharyngeal reflux treatment: a systematic review of 1483 patients
- Change of acoustic parameters before and after treatment in laryngopharyngeal reflux patients
- Healthcare for the Vocal Performing Artist
- Compliance and Quality of Life in Patients on Prescribed Voice Rest
- GERD: Foods to Avoid & Foods That Help
- 7 Foods To Eat During Acidity- From A Mum Who Said Goodbye To Acid Reflux
- This Is What Your Heartburn Really Means